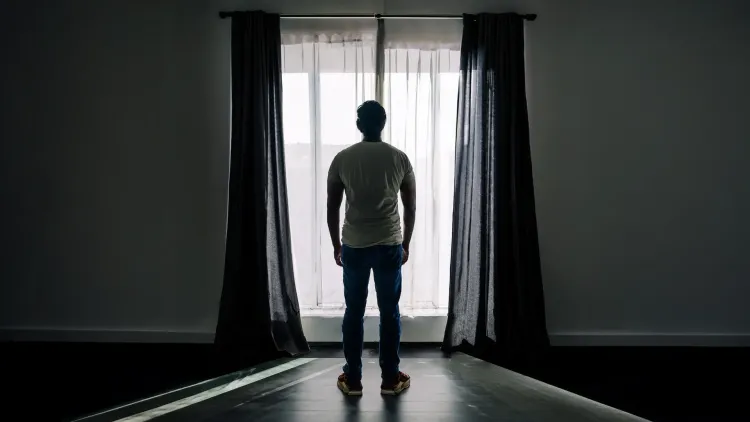
Could Depression and Bipolar Disorder After 40 Indicate Dementia Risk?
Synopsis
Key Takeaways
- Mood disorders after 40 may indicate future cognitive decline.
- Early recognition of late-life mood disorders (LLMDs) is crucial.
- About 50% of participants with LLMDs have abnormal tau proteins.
- Symptoms can precede cognitive decline by an average of 7.3 years.
- Timely intervention could lead to better outcomes for individuals.
New Delhi, June 9 (NationPress) Mood disorders such as depression, bipolar disorder, or mania that emerge after the age of 40 may signify more than just mental health issues; they could indicate the onset of motor or cognitive symptoms associated with various neurodegenerative conditions, as highlighted by a recent study.
Accumulating evidence points to these late-life mood disorders (LLMDs) potentially serving as precursors for neurodegenerative diseases, including dementia, even manifesting years before cognitive decline or memory loss becomes evident, according to researchers from the National Institutes for Quantum Science and Technology (QST) in Japan.
The findings, published in Alzheimer's & Dementia: The Journal of the Alzheimer's Association, investigated the presence of abnormal tau protein, which is a characteristic feature of multiple neurodegenerative disorders, in the brains of 52 individuals with LLMDs compared to 47 healthy controls.
Utilizing advanced brain imaging methods, the researchers applied positron emission tomography (PET) scans with two distinct tracers to identify various forms of tau protein and amyloid beta accumulation. They also analyzed brain tissue samples from 208 autopsy cases to explore the correlation between late-life mood symptoms and the later emergence of neurodegenerative diseases.
Results indicated that around 50 percent of participants with LLMDs exhibited tau accumulation in their brains, in contrast to about 15 percent of the healthy control group.
Furthermore, nearly 29 percent of those with LLMDs had detectable amyloid deposits, compared to just 2 percent of controls. Autopsy results corroborated these findings, revealing a significantly higher occurrence of various tau protein-related pathologies in individuals who had experienced late-life mania or depression.
“Given that most participants with LLMDs in our study experienced no or minimal cognitive decline, these outcomes support the notion that neurodegenerative diseases, including Alzheimer’s and other tau-related pathologies, can manifest initially through psychiatric symptoms,” stated Dr. Shin Kurose from QST.
Additionally, many participants showed tau accumulation in the frontal regions of the brain, which are essential for emotional regulation and cognitive abilities.
The research demonstrated that these abnormal proteins could be identified years prior to the standard cognitive symptoms of dementia. As indicated by the autopsy cases, mood symptoms appeared on average 7.3 years before cognitive or motor symptoms.
Early recognition of late-life depression and bipolar disorder could enable timely intervention with disease-modifying treatments, the research team concluded.