How Does Childhood Trauma Impact Long-Term Mental Health?
Synopsis
Key Takeaways
- Childhood adversity is linked to lifelong mental health vulnerability.
- Early life trauma can alter brain structure and immune function.
- Identifying inflammatory markers opens new treatment avenues.
- A shift towards precision medicine is essential in psychiatric care.
- Mood disorders like MDD and BD significantly impact global health.
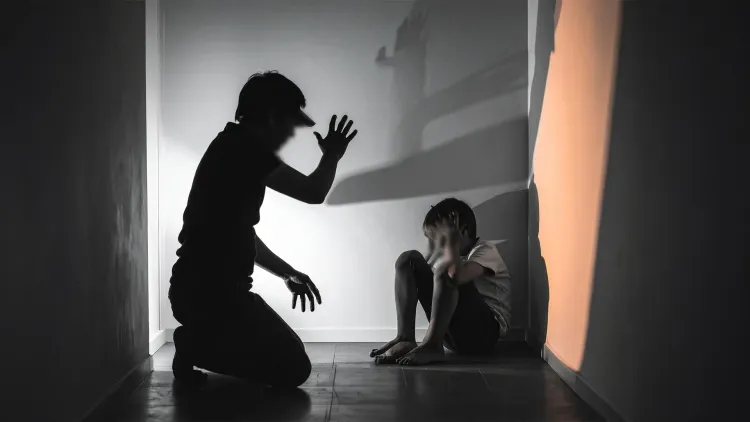
New Delhi, June 10 (NationPress) Childhood adversity can significantly influence lifelong susceptibility to psychiatric disorders and other neurological impacts, as demonstrated by a recent study.
The research indicates that early life challenges become biologically ingrained, leading to enduring alterations in brain structure and immune function.
According to Sara Poletti, a senior researcher at IRCCS Ospedale San Raffaele Milan, Italy, "The immune system does more than combat infections; it is vital in shaping our mental health over a lifetime."
“Childhood trauma can fundamentally reconfigure these immune responses, resulting in increased susceptibility to conditions such as depression, bipolar disorder, and other psychiatric issues many years later,” she elaborated.
By pinpointing specific inflammatory markers linked to childhood trauma, the study proposes potential targets for innovative therapeutic approaches.
The research advocates for a precision medicine strategy to shift psychiatric care from merely managing symptoms to addressing the underlying biological causes.
This study, published in the journal Brain Medicine, emphasizes the potential of using an immunomodulatory agent (interleukin 2) in treating mood disorders.
The World Health Organization (WHO) recognizes mood disorders as a major contributor to global disability, morbidity, and mortality. Among these, major depressive disorder (MDD) and bipolar disorders (BD) are the most common and debilitating.
The lifetime prevalence rates are approximately 12% for MDD and 2% for BD.
Recent findings suggest a growing link between immune dysregulation and mood disorders, particularly emphasizing the role of the inflammatory response system (IRS), which may be a critical pathological factor in these conditions.
“I strive to further clarify the immune system's role and its interaction with environmental factors in psychiatric disorders,” Poletti noted.
Her vision includes formulating strategies to prevent mental illnesses, especially for individuals with histories of trauma, marking a shift from reactive to proactive psychiatric care.