What Causes the Severe Weight Loss in Cancer Patients?
Synopsis
Key Takeaways
- Cachexia affects a significant number of cancer patients.
- Disrupted communication between the brain and liver is a key factor.
- Therapies targeting the vagus nerve show potential for improving outcomes.
- Current studies indicate a possible shift in treatment approaches for impacted patients.
- Understanding brain-body communication is crucial in health management.
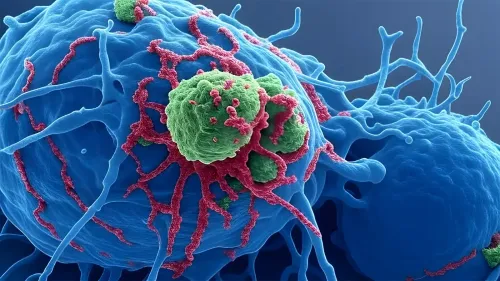
New Delhi, Aug 8 (NationPress) A recent study indicates that the alarming weight loss observed in cancer patients, which can often lead to fatalities, may stem from disrupted communication between the brain and the liver. Approximately one-third of deaths related to cancer are attributed to cachexia, an incurable metabolic disorder characterized by significant weight loss, including the reduction of muscle mass and body fat.
This condition not only contributes to resistance against therapy but also heightens mortality rates among those affected.
Researchers from the Weizmann Institute of Science in Israel and the University of Texas MD Anderson Cancer Center in the US have identified that one of the primary causes of this weight loss is impaired communication between the brain and the liver.
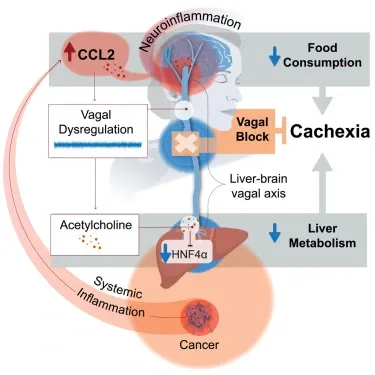
When the vagus nerve, a crucial pathway for brain-liver interaction, is disrupted due to inflammation triggered by cancer, it leads to metabolic damage in the liver and the emergence of this life-threatening syndrome.
The occurrence of cachexia in cancer patients can be as high as 85% in certain cancers, with the highest rates seen in pancreatic and lung tumors, according to the team led by Dr. Naama Darzi at Weizmann and Dr. Aliesha Garrett at MD Anderson.
The findings, published in the journal Cell, revealed that specifically blocking the right vagus nerve—using noninvasive techniques—could prevent the onset of cachexia in mice, improve their response to chemotherapy, and enhance their overall health and longevity.
This innovative method is currently undergoing clinical trials and may pave the way for improved patient quality of life and survival rates, the research team noted.
Given that the technique utilizes technologies already approved for clinical application, it could soon be accessible to patients.
This study not only opens new avenues for cancer treatment but also underscores the significant role that brain-body communication plays in our overall health and disease, the researchers emphasized.