How is Inflammation Connected to Frailty, Social Deprivation, and Heart Disease Risk in Women?
Synopsis
Key Takeaways
- Chronic inflammation is linked to increased risk of frailty and cardiovascular disease.
- 10 inflammatory proteins identified as risk factors.
- Social deprivation impacts health through chronic inflammation.
- Potential dual approach for public health: medical and social strategies.
- Findings validated in diverse populations.
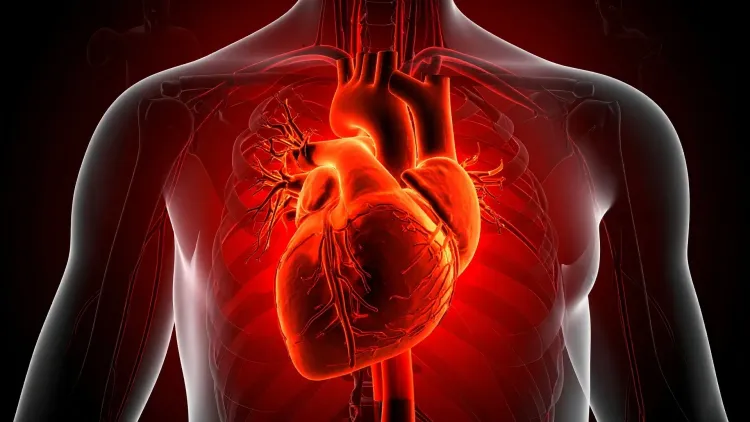
New Delhi, Aug 5 (NationPress) Chronic inflammation may be linked to a heightened risk of frailty, social deprivation, and cardiovascular disease (CVD), according to a recent study.
The research, published in the journal Communications Medicine, examined 74 inflammation-associated proteins in blood samples from over 2,000 women aged between 37 and 84 years, investigating how inflammation correlates with frailty, social disadvantage, and CVD risk.
The team discovered 10 inflammatory proteins that were correlated with both frailty and residing in deprived areas.
Among these, four proteins involved in cellular signaling, growth, and movement—TNFSF14, HGF, CDCP1, and CCL11—were also found to be linked to an increased risk of cardiovascular disease.
"To gain deeper insights into how frailty and deprivation contribute to heart disease, we employed a data-driven strategy, screening a wide array of inflammatory proteins in the blood. By pinpointing overlapping biological markers associated with both social and health vulnerabilities, we unveiled a potential shared pathway linking these risk factors," stated Dr. Yu Lin, Research Associate in the Department of Twin Research and Genetic Epidemiology at King's College London.
One particular protein, CDCP1, showed a significant connection to future heart disease occurrences, such as narrowed or blocked arteries. These results imply that certain inflammatory proteins could function as a biological connection between social inequality, aging, and heart disease.
Furthermore, the research team validated their findings in an independent cohort of women to confirm consistency across diverse populations.
"Frailty, social disadvantage, and heart disease frequently coexist, yet the biological mechanisms connecting them remain unclear. Our results indicate that the stresses of socioeconomic challenges may trigger detrimental inflammation that adversely affects health over time," remarked Dr. Cristina Menni, Senior Lecturer in Molecular Epidemiology at King's College London.
"If validated, this could lead to innovative methods for disease prevention, not only through medical interventions aimed at reducing inflammation but also by implementing social policies to tackle health inequalities," she added.
The proteins identified in this study may also act as biomarkers, assisting clinicians in recognizing individuals at a higher risk of heart disease.
The findings propose that a dual approach to public health could effectively diminish CVD risk among vulnerable populations, merging medical strategies that mitigate inflammation with more comprehensive social policies addressing inequality.










