Can Novel CAR-T Therapy Revolutionize Treatment for Hard-to-Treat Cancer?
Synopsis
Key Takeaways
- HSP-CAR30 shows unprecedented efficacy in treating refractory CD30+ lymphoma.
- Achieved a 100% overall response rate in the trial.
- 50% of patients reached complete remission.
- 60% of responders maintained remission after a median of 34 months.
- No significant toxicities were reported during the study.
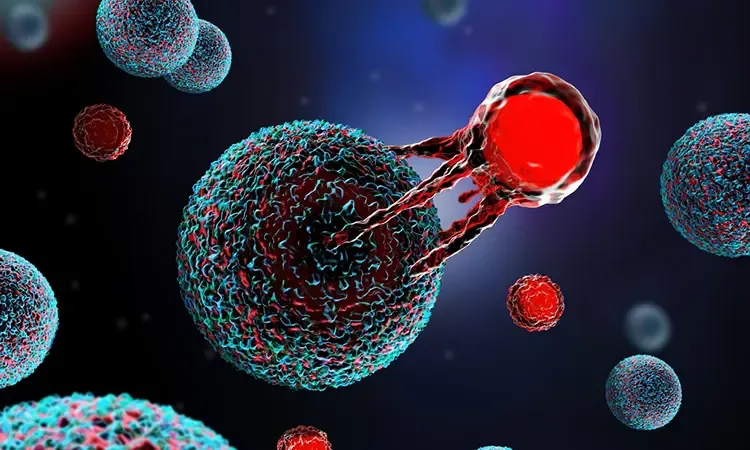
New Delhi, April 29 (NationPress) A group of researchers from Brazil has pioneered a groundbreaking CAR-T cell therapy demonstrating significant efficacy in patients suffering from a refractory form of lymphoma, which affects the lymph nodes, spleen, and bone marrow. HSP-CAR30 is the inaugural European CAR-T30 study to successfully complete its preliminary phase.
Findings from the Phase I trial, published in the journal Blood, indicate that this innovative therapy, targeting the CD30 protein, has exhibited remarkable effectiveness in patients with refractory CD30+ lymphoma.
The therapy also encourages the proliferation of memory T cells, resulting in enduring responses and enhanced clinical outcomes for those treated.
Dr. Javier Briones, Head of Hematological Oncology at the Sant Pau Research Institute (IR Sant Pau), remarked, "The most striking aspect is the 100 percent overall response rate, a rarity among patients who have undergone multiple treatment regimens. Furthermore, 50 percent of participants attained complete remission, indicating that the disease was undetectable in imaging and clinical assessments."
Approximately 60 percent of patients who achieved a complete response maintained their remission status without signs of relapse after a median follow-up period of 34 months.
Briones emphasized, "This is vital because it suggests that the persistence of CAR-T cells within the body has a true and lasting effect on the condition, which is precisely our objective with such therapies."
While CAR-T cell therapies have proven to be a promising alternative for treating B-cell leukemias and lymphomas, their use in CD30+ lymphomas has been restricted due to the lack of persistence of modified cells and a high relapse rate among patients.
The Phase I trial included 10 patients with relapsed or refractory classical Hodgkin lymphoma or CD30+ T-cell lymphoma, yielding exceptionally positive results.
No dose-limiting toxicities were reported.
One of the most noteworthy discoveries from the study was the significant in vivo persistence of CAR30+ cells, which were still detectable in 60 percent of evaluable patients one year post-infusion.