High-Definition Ultrasound for Rapid Prostate Cancer Diagnosis: Research Findings
Synopsis
Key Takeaways
- Micro-ultrasound is a cost-effective alternative to MRI.
- It can speed up the diagnosis process.
- Similar detection rates of cancer between both biopsy methods.
- Less need for multiple hospital visits.
- Clinicians can be trained easily to use microUS technology.
New Delhi, March 23 (NationPress) An international clinical trial revealed on Sunday that biopsies guided by high-definition ultrasound are just as effective as those utilizing MRI for diagnosing prostate cancer.
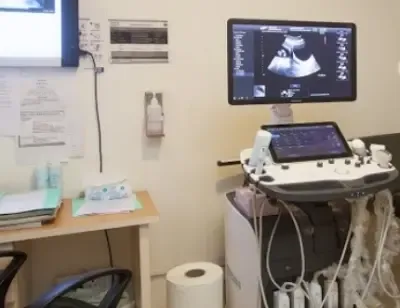
This innovative technology, known as micro-ultrasound, is more cost-effective and user-friendly compared to MRI.
“It has the potential to accelerate diagnosis, lessen the necessity for multiple hospital visits, and allow MRI machines to be used for other purposes,” the researchers stated. The findings were shared at the European Association of Urology Congress in Madrid and published in the JAMA journal.
This is the first randomized trial comparing micro-ultrasound (microUS) guided biopsy with MRI-guided biopsy for prostate cancer. The study involved 677 men who underwent biopsy procedures at 19 hospitals across Canada, the USA, and Europe.
Half of the participants received MRI-guided biopsies, a third underwent microUS-guided biopsies followed by MRI-guided biopsies, while the remaining participants received only microUS-guided biopsies.
MicroUS successfully detected prostate cancer with the same efficacy as MRI-guided biopsies, demonstrating similar detection rates across all trial groups.
Even in the group receiving both biopsy types, the microUS detected the majority of significant cancers, as noted by the authors.
MRI-guided biopsy involves a two-step procedure (the MRI scan followed by the ultrasound-guided biopsy), necessitating multiple hospital visits and requiring specialist radiological expertise to interpret MRI images and integrate them with ultrasound.
Micro-ultrasound operates at a higher frequency than traditional ultrasound, resulting in images with three times the resolution, capturing detail akin to MRI scans for targeted biopsies.
Clinicians, including urologists and oncologists, can be trained easily in this technique and image interpretation, especially if they have prior experience with conventional ultrasound.
Laurence Klotz, Professor of Surgery at the University of Toronto’s Temerty Faculty of Medicine, emphasized that microUS can provide diagnostic accuracy comparable to MRI, which is revolutionary.
“This enables a one-stop solution where patients can be scanned and biopsied immediately if necessary. There’s no toxicity, no exclusions, and it’s significantly cheaper and more accessible. Plus, it frees up MRIs for other essential uses,” he added.