Ultrasound-Activated CAR T-Cell Therapy for Extended Tumor Elimination
Synopsis
Key Takeaways
- New EchoBack CAR T-cells can attack tumors for five times longer than traditional methods.
- Ultrasound serves as an activation mechanism for targeted cancer destruction.
- Potential to treat tumors typically resistant to immunotherapy.
- Reduces the need for frequent hospital visits for patients.
- Demonstrated superior performance in lab models against various cancer types.
New Delhi, April 4 (NationPress) US researchers have developed a groundbreaking ‘smart’ immune cell that, when activated by ultrasound, can continuously detect and eliminate cancer cells over extended durations.
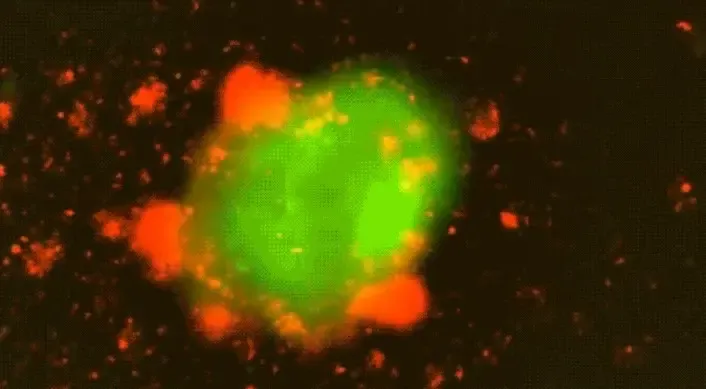
The EchoBack CAR T-cell, crafted by biomedical engineers at the University of Southern California (USC), has the potential to revolutionize cancer immunotherapy.
The findings, published in the scientific journal Cell, reveal that these innovative EchoBack CAR T-cells can target tumor cells for five times longer than conventional CAR T-cells, making it suitable for medical applications.
These cells can be precisely directed to attack tumors using focused ultrasound, potentially enhancing both safety and efficacy of the treatments.
This new strategy may address significant challenges in treating tumors typically unsuitable for immunotherapy while protecting healthy tissues, according to the research team.
In contrast to the first-generation, ultrasound-activated CAR T-cells, which typically only engage with cancer cells for up to 24 hours before becoming inactive, lead author Longwei Liu, an Assistant Professor at the USC Viterbi School of Engineering, explained that the EchoBack CAR T-cells are activated directly at the tumor site by ultrasound.
Once activated, these CAR T-cells can persist in their efforts to locate and destroy cancer cells for at least five days without becoming fatigued.
“Patients using the first-generation cells may need daily hospital visits for treatment. However, with this new innovation, treatment can be reduced to once every two weeks, or even less frequently,” Liu noted.
The research team utilized ultrasound technology as an “on switch” for the CAR T-cells—engineered to respond to a brief 10-minute pulse of ultrasound, triggering the cells to sense nearby cancer cells.
The new CAR T-cells were examined in lab experiments using mouse models with various tumor cells, including prostate cancer and glioblastoma.
“Our results clearly indicate that the ultrasound-controlled CAR, combined with two rounds of ultrasound stimulation, significantly outperformed standard CAR T-cells,” Liu remarked. “Furthermore, while the standard CAR became exhausted and dysfunctional after repeated challenges with tumor cells, our ultrasound-controlled CAR maintained superior function, reduced exhaustion, and enhanced cancer cell killing capability.”