Waist Circumference Emerges as Key Risk Factor for Obesity-Related Cancer in Men

Synopsis
Key Takeaways
- WC is a stronger risk marker than BMI for men.
- Visceral fat accumulation is more harmful.
- Data analyzed from 339,190 individuals.
- High WC remains a risk factor after adjusting for BMI.
- Gender differences in fat distribution are significant.
New Delhi, March 23 (NationPress) Waist circumference (WC) is found to be a more significant risk marker than BMI for the onset of obesity-related cancers in men, according to a recent study. BMI serves as an indicator of body size but fails to convey details about fat distribution. In contrast, waist circumference serves as a more accurate proxy linked to abdominal fat accumulation.
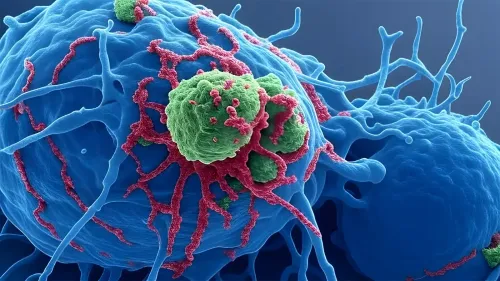
“This differentiation is vital since visceral fat, which gathers around the abdominal organs, is metabolically more active and has been associated with negative health consequences, including insulin resistance, inflammation, and abnormal lipid levels,” explained the study conducted by Dr. Ming Sun, Dr. Josef Fritz, and Dr. Tanja Stocks.
As a result, individuals with identical BMI scores may face varying cancer risks due to differences in fat distribution, they pointed out.
The research examined data from 339,190 participants sourced from various Swedish populations, who underwent health evaluations that included assessments of both BMI and WC from 1981 to 2019 (61 percent were objectively measured, and 39 percent were self-reported, with a mean age of 51.4 years). Cancer diagnoses were retrieved from the Swedish Cancer Register.
The authors computed relative risks connected to obesity-related cancers for both WC and BMI, accounting for various factors that could sway the outcomes, such as age, smoking habits, and sociodemographic elements like education level, income, country of birth, and marital status.
During a median follow-up period of 14 years, 18,185 cases of recognized obesity-related cancers were documented.
Even after taking BMI into account, a high WC continued to be a risk factor for obesity-related cancer in men. This indicates that the increased risk linked to abdominal fat is specific and cannot be attributed solely to high body size, as indicated by BMI.
In women, the associations were less pronounced and showed similarities for both WC and BMI.
“A reasonable explanation is that men are more prone to store fat viscerally, while women tend to accumulate more subcutaneous and peripheral fat,” the authors noted in the Journal of the National Cancer Institute.
Incorporating hip circumference into risk models may offer additional insights into this gender difference and strengthen the correlation between WC and cancer, particularly for women, they concluded.