Odisha Government Signs MoU to Launch Ayushman Bharat
Synopsis
Key Takeaways
- Odisha has signed an MoU for Ayushman Bharat.
- Implementation will provide Rs 5 lakh coverage per family.
- Approximately 1.03 crore families will benefit.
- Union Health Minister noted 45% of India's population is covered.
- Scheme will improve access to 29,000 hospitals.
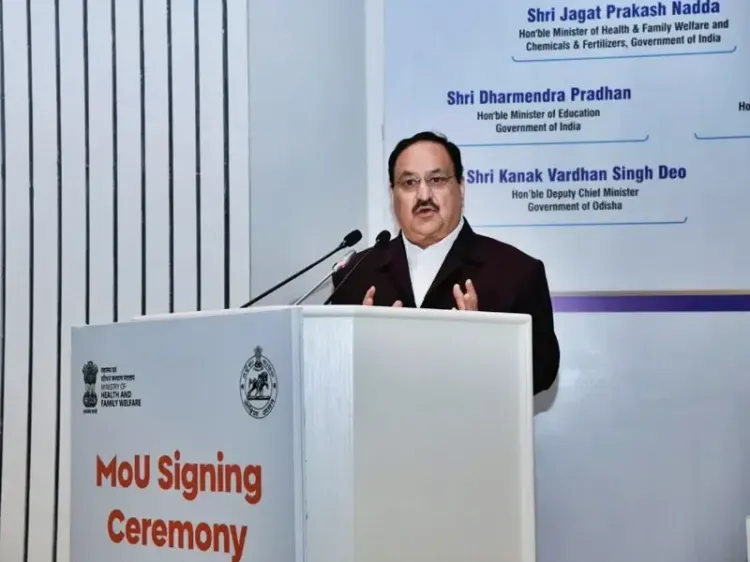
Bhubaneswar, Jan 13 (NationPress) The Health & Family Welfare department of Odisha formally entered into a Memorandum of Understanding (MoU) with the National Health Authority under the Union Health Ministry for executing the Ayushman Bharat initiative within the state.
With this, Odisha marks its position as the 34th state to adopt the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY).
The implementation will synergize with the ongoing Gopabandhu Jan Arogya Yojana (GJAY) in Odisha.
This initiative will offer a financial cover of Rs 5 lakh per family annually, with an additional Rs 5 lakh for female members.
Approximately 1.03 crore families are expected to benefit from the integrated scheme, with 67.8 lakh families receiving support from the Union government.
During the event, Union Health Minister J.P. Nadda stated: "Today is a historic day for Odisha. AB PM-JAY is not only the world's largest health coverage scheme but also the fastest to be executed since its inception."
He noted that nearly 45 percent of India's population benefits from the AB PM-JAY scheme.
Furthermore, J.P. Nadda announced that the Ayushman Vay Vandana Card, introduced in October 2024, is set to assist around 6 crore individuals aged 70 and older.
Since the launch of AB PM-JAY, there have been 8.19 crore hospital admissions, with a total expenditure of Rs 1.13 lakh crore aimed at providing healthcare to the underprivileged.
Quoting a recent Lancet study, he revealed that AB PM-JAY has enhanced access to healthcare for cancer patients by 33 percent.
On this occasion, Odisha's Chief Minister Mohan Charan Majhi remarked: "Residents of our state, previously receiving treatment at around 900 empaneled hospitals, will now enjoy access to cashless and quality healthcare at over 29,000 government and private empaneled hospitals."
He emphasized that the merged schemes of GJAY and ABPM-JAY will collectively benefit approximately 4.5 crore people in Odisha through a single card.
"The AB PM-JAY, recognized as the world’s largest health assurance scheme, was initiated in 2018 by PM Modi, covering health services for over 50 crore people in the nation. However, due to political circumstances, many in Odisha were excluded from it under the previous state government. To rectify this, the state government decided to implement ABPM-JAY promptly," Majhi stated.
He also mentioned that nearly one crore families in Odisha are already receiving health assurance through the state’s Gopabandhu Jan Arogya Yojana.
CM Majhi added that each month, 1.50 lakh patients receive cashless treatment worth approximately Rs 350 crore at empaneled private hospitals.
"Nonetheless, there are certain limitations. Currently, beneficiaries can access cashless treatment only at 900 empaneled private hospitals. Additionally, those residing outside the state are excluded from this scheme. These issues will be resolved with the rollout of ABPM-JAY, allowing beneficiaries to access cashless treatment at more than 29,000 government and private hospitals across India," concluded CM Majhi.









