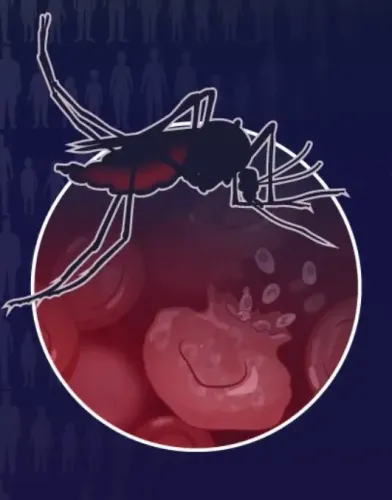
How Do TB Bacteria Protect Themselves From Antibiotics?

Synopsis
Key Takeaways
- Mycobacterium tuberculosis alters its lipid coating to survive antibiotics.
- TB remains a global health crisis with millions affected.
- The study provides insights into the bacteria's drug tolerance mechanisms.
- Innovative strategies are needed to combat TB effectively.
- Combining old drugs with membrane-weakening molecules may enhance treatment.
New Delhi, Dec 3 (NationPress) The bacterium Mycobacterium tuberculosis, responsible for the highly contagious disease Tuberculosis (TB), has shown an ability to evade antibiotic treatments and prolong its survival by altering its outer lipid coating, according to a recent investigation led by scientists from the Indian Institute of Technology (IIT) Bombay.
Despite the availability of effective antibiotics and extensive vaccination efforts, TB continues to claim lives across the globe.
In 2024, there were 10.7 million new TB cases worldwide, resulting in 1.23 million deaths, with India facing one of the largest burdens—over 2.71 million cases reported that year.
The findings, published in the Chemical Science journal, reveal that the bacteria's ability to tolerate drugs is linked to their membranes, which serve as complex barriers comprising mainly fats or lipids.
The research team cultured the bacteria under two scenarios: one simulating an active infection with rapid division, and the other reflecting a dormant state akin to latent infections.
Upon exposure to four standard TB medications—rifabutin, moxifloxacin, amikacin, and clarithromycin—the team discovered that the drug concentrations required to inhibit 50 percent of bacterial growth were two to ten times greater in dormant bacteria compared to active ones.
In essence, “the same medication that proved effective during the disease's early stages would need to be administered at significantly higher concentrations to eliminate the dormant or persistent TB cells. This phenomenon was not attributed to genetic mutations, which typically account for antibiotic resistance,” stated Prof. Shobhna Kapoor from IIT-Bombay's Chemistry Department.
The lack of genetic mutations associated with antibiotic resistance in these bacteria confirmed that the diminished drug sensitivity was likely related to their dormant state and primarily to their membrane structures rather than genetic alterations.
Additionally, the researchers identified over 270 unique lipid molecules within the bacterial membranes, revealing distinct differences between active and dormant cells.
Active bacteria exhibited loose, flexible membranes, while dormant ones possessed rigid, tightly organized structures, indicating a defensive mechanism.
“For decades, TB research has focused on proteins,” noted Kapoor. “However, lipids have long been perceived as passive elements. We now understand that they play a vital role in aiding the bacteria's survival and resistance to drugs,” she added.
The study also revealed that rifabutin could easily penetrate active cells but struggled to breach the outer membrane of dormant cells.
“The rigid outer layer acts as the primary barrier, constituting the bacterium's first and strongest defense,” Kapoor explained.
If this outer membrane obstructs antibiotics, there is potential for enhancing drug efficacy by weakening it.
“Even older antibiotics could become more effective if paired with a molecule that loosens the outer membrane,” Kapoor remarked, emphasizing that this strategy could restore bacterial sensitivity to the drugs without allowing for the development of permanent resistance.